Introduction
A cavity filled with mucous is called mucocele.1 Oral mucoceles (OM) are swellings associated with minor salivary glands of the oral cavity. Minor salivary glands are present in most parts of the oral cavity except gingiva. The prevalence is most common in lower lip and rarely on ventral surface of the tongue (1.9to 10.3%).2, 3 B More et al study showed OM were more prevalent in the age group of 15-24 years, lesions occurred in 51.72% of males and 48.28% of females, with a ratio of 1.07:1.4 Blandin and Nuhn salivary glands are bilaterally embedded in the muscles of anterior ventral tongue region and are mainly mucous-secreting glands.3 Mucoceles are classified into two types first is extravasation type in which mucus is extravasated in connective tissue region and second is retention type, in this mucus collects inside the gland lumen.1, 5 Most common etiological factor of OM is trauma which can cause rupture of the gland duct and extrvasation of the ductal secretions in the surrounding connective tissue (92%) or blockage of the gland duct (8%).1, 5, 6 Clinically they may appear as vesicullobullos swelling or a nodule and size may range from few millimeters to centimeters. Consistency can be flabby and sometimes there is history of fluid discharge from the lesion.1, 3 The extravasation type OM triggers inflammatory reaction, are not lined by epithelial lining and present as pseudocyst. It is seen mostly in young patients on labial mucosa, buccal mucosa and retromolar area.5 Retention type cyst may occur due to duct obstruction by sialolith or strictures and commonly seen in older age group, on upper lip, hard palate or floor of mouth(Ranula).7 The tongue has three sets of minor salivary glands; Weber glands on the lateral border of the tongue, Von Ebner glands around circumvallated and foliate papillae, and Blandin-Nuhn glands in the deep portion of the ventral tongue. Blandin and Nuhn glands are rarely associated with mucocele because of its deep seated location protected by muscles from any traumatic injury. Blandin and Nuhn glands are non-encapsulated glands and drain near lingual frenum.5, 6 This case reports a rare presentation of a large Blandin and Nuhn glands mucocele (BNGM) with review of literature.
Case Report
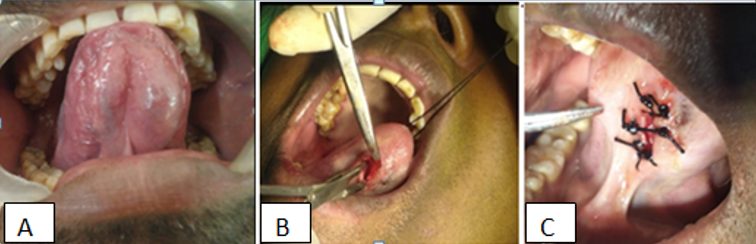
A 37 year old male patient reported with complaint of swelling, discomfort due to swelling on tongue since four years. The swelling gradually increased to present size with negative history of fluid discharge. Medical and surgical history was not significant. Examination showed a large sessile, soft and fluctuant swelling of size approximately 2.5cm x 1.5 cm (Figure 1 A) on ventral surface of the tongue with smooth surface, non tender with negative history of bleeding. Provisional diagnosis BNM was considered with differential diagnosis of minor salivary gland tumor, lipoma and vascular pathology. Informed consent was obtained from the patient. Clear viscous fluid was aspirated from the lesion which suggested for clinical diagnosis of mucocele. Surgical excision was planned for the removal of the lesions. Surgical site preparation was done under local anaesthesia, longitudinal incision was made on the mid part of the lesion and careful dissection was performed, lesion punctured and thick mucus was drained. After marsupialization, multiple sutures were given with 2.0 silk around the lesion with the mucosa. (Figure 1 B, C) Follow up after three days was uneventful and unfortunately patient did not report for further follow up.
Discussion
The glands of Blandin-Nuhn (BN) consist of seromucous, mucous acini, located near the midline of the ventral tip of the tongue. BN glands are nonlobulated, 1-8mm wide, 12-25 mm deep in muscles. These glands drain near lingual frenum through 5-6 small ducts.1 OM commonly occurs on lower lip (77.9%) followed by floor of the mouth and tongue (15.6%)2, 8 BNGM is uncommon, with 9.6 to 18.3% occurrence found among all oral mucoceles. A Brazilian study found 8.3% mucoceles on ventral aspect of the tongue in the pediatric age of upto 15 years and can be present as congenital mucolcele.9, 10 Its size is generally less than 2cm but BNM can be large with long axis over 5 cm. Although the size of the gland is small that is 8mm. BNM are largely of extravasation type which suggests trauma as etiology. Large BNMC can be associated with suffocation, discomfort, dysphagia difficulty in feeding, and speech.1, 2, 8 Colour of these lesions may vary from blue to the normal pink and blue colour may occur due to tissue cyanosis, vascular congestion with stretched overlying tissue and translucent accumulated fluid. Its colour also depends on the size, proximity to the mucosa and the elasticity of the overlying tissue of the lesion.11 Delay in visit by the patient for the lesion, may be attributed to asymptomatic lesion.1 Clinically these mucoceles are placed parallel to lingual frenum. Differential diagnosis includes vascular lesions, squamous papillomas, mucoepidermoid carcinoma. lipoma, benign or malignant salivary gland neoplasms, irritational fibroma, soft tissue abscess, pyogenic granuloma, etc. The superficial mucoceles may be confused with cicatricial pemphigoid, bullous lichen planus, etc. Bluish colour, change in size, and fluid consistency and location will help in reaching the diagnosis of BNGM. Although diagnosis is mainly clinical but better visualization of the lesion may be obtained by ultrasonography or computed tomography and magnetic resonance imaging. Fine-needle aspiration is helpful in differentiating mucocele from angiomatous lesions. Chemical analysis of fluid may show high amylase and protein content.4, 8 CT scan appearance usually present as homogenous and well defined lesion, MRI shows a low intensity images on T1-weighted images (TIWI) and high intensity and fat suppression on T2WI images.11, 12
Treatment of choice for BNGM is complete en bloc surgical excision under local anesthesia, if the lesion is small and if required than under general anesthesia. Surgery for asymptomatic lesions prevents complications associated with increase in size. The BN glands must be excised and lingual nerves, vessels, Wharton’s duct, sublingual gland should be preserved. A longitudinal incision parallel to lingual frenum and 5 mm away from midline is given, mucus is drained and it is than sutured with absorbable stiches. Recurrence of the lesion may occur due to inflammatory induced adhesions. Histopathological examination may reveal a well circumscribed lesion on top of mucous filled with a colourless mucoid material containing proteins and large histiocytes. The histopathologic aspect can show acute inflammation intermingling with the mucus and mature lesions with scarce amounts of mucus and connective tissue fibrosis. Presence of salivary gland tissue and sialomucin are diagnostic feature of histopathological examination.4, 8 Other recommended treatment options for large lesions are cryotherapy, laser, “micromarsupialisation,” and intralesional steroid injection, intralesional ethanol injection, scleorising agent OK- 432 injection . The cystic cavity may be filled with rubber impression or alginate material to improve the visual access for excision.1, 8, 10 Baurmash recommends complete unroofing of the lesion which gives better accessibility for removal of the glands present and it should be followed by uneventful healing. Recurrence can occur after marsupialization after healing of the drainage site. To avoid recurrence glands including smaller one should be removed upto the muscle plane.9, 13, 14 Mostly BNGM are extravasation type and not lined by epithelium and lesion contain mucin, walls of the lesion may consists of granulation tissue with leukocytes and phagocytes. Special stains such as mucicarmine and Halcian blue are helpful in identifying mucin that is present freely in tissues or in the foamy macrophages. Histology shows the seromucous acini glands are present in their anterior portion and of mucous acini capped by seromucous demilunes in their posterior portion.1, 9, 13
Conclusion
Mucoceles of Blandin and Nuhn affect ventral surface of the tongue adjacent to midline. Blandin and Nuhn gland associated mucocele should be considered in differential diagnosis of the swellings on ventral surface of the tongue. Surgical treatment is the most common approach for management for the lesion. These lesions may cause discomfort, feeding difficulties and suffocation. Thus, timely diagnosis, management and follow up should be done for swelling of the ventral surface of the tongue to prevent later complications.