Background
An oroantral perforation is an unusual communication between the oral cavity and maxillary sinus. Extraction of maxillary premolars and molars, cysts, tumours, osteomyelitis are the common aetiologies of Oroantral communication (OAC).1
Table 0
|
Oroantral fistula size |
Treatment plan |
|
Measuring < 3mm |
Close spontaneously |
|
Measuring > 5mm |
Surgical intervention |
Several techniques have been reported to close the OAF which include buccal advancement flaps, palatal rotation, tongue flaps and buccal fat pad (BFP).2, 3 Of all these techniques only soft tissue closure is achieved while completely neglecting the bony defect. However, it's important to note that the underlying bony defect carries its own consequences for prosthetic rehabilitation.
In this present case, we showcase the successful application of three layered closure by using a) BFP b) Guided Tissue Regeneration (GTR) membrane and C) sticky bone graft made of (Autogenous and Xeno graft with i-Platelet Rich Fibrin (PRF)) coupled with closure utilizing buccal advancement flap and collagen membrane for OAF reconstruction.
Procedure
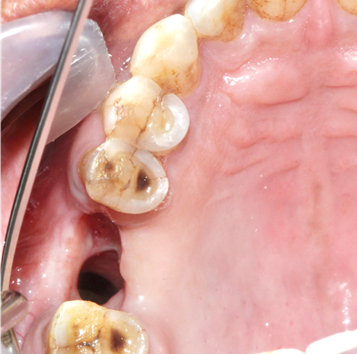
54 year old male patient, presented with pain and nasal passage of fluids during mastication, following the extraction of his upper right back tooth six months prior. Clinical examination revealed a fistulous opening in the right maxillary first molar region measuring approx. 1-1.5cm with an evident bony defect along the maxillary molar region (Figure 1).
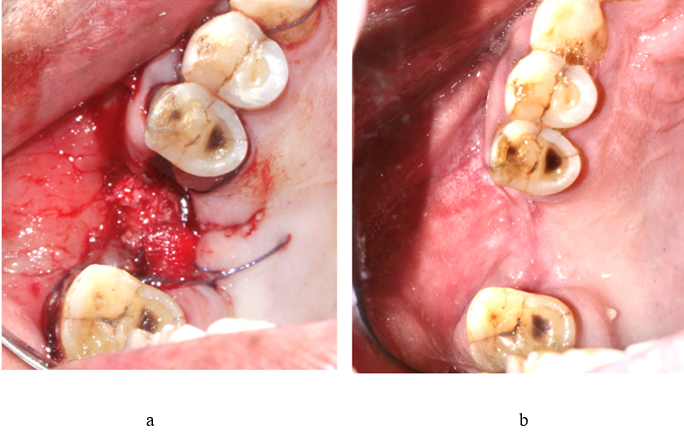
Figure 2
a. Excision of fistula b. Fistula track c. Harvesting buccal fat pad in continuity d. Sticky bone preparation e. Adaptation of sticky bone over the defect
The Procedure was performed under local anaesthesia (2% lignocaine with 1:80,000 adrenaline) involving excision of fistulous tract in a circumscribed manner (Figure 2 a). Blunt dissection was carried out to harvest buccal fat pad which was sutured over the defect (Figure 2 c). Followed by, GTR membrane was placed and sutured to serve as a barrier on the BFP.
Preparation of sticky bone: Autogenous bone graft was harvested from the external oblique ridge region and Xenograft granules were mixed in 1:1 ratio. 20ml of patient venous blood was drawn and then centrifuged for 3 minutes at 700 rpm to obtain iPRF. This was mixed with bone graft and left for 10 minutes for agglutination. The two components were firmly united in a compound with gelatinous consistency to form a sticky bone (Figure 2 d).
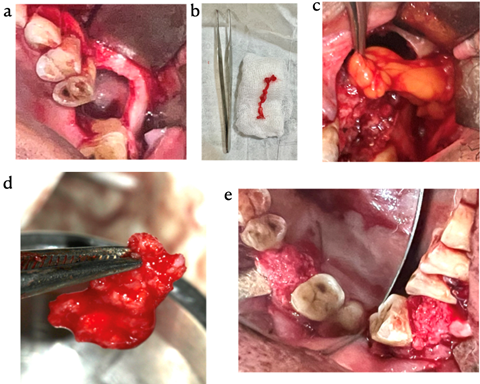
This sticky bone, was moulded and adapted over the GTR membrane to cover the bony defect (Figure 2 e.). Subsequently, collagen plug and buccal advancement flap was sutured to prevent the graft exposure in the oral cavity (Figure 3 a). This way, 3-layered closure was performed to reconstruct the bony as well as soft tissue defect.
Discussion
Oroantral fistula closure requires consideration of various factors, including defect size, duration since development, infection and presence of foreign bodies. The fundamental concept is to achieve the total closure and establish a seal between the maxillary sinus and the oral cavity for sufficient nasal outflow in order to keep out from infection. Traditional flap closure techniques may result in vestibular depth loss, requirement for a second operation, wound dehiscence.4
Our idea of three-layer closure is based on the studies of Er et al. and Weinstock et al.5, 6 Er et al. observed wound dehiscence in 20% of cases after two-layered closure. BFP has emerged as a reliable option for closure of oral defects due to its reliability, ease of harvesting, excellent blood supply and can cover upto 10cm X cm and 6mm thickness. 7 Tideman et al. have shown the BFP alone can self-epithelialize within 3-4 weeks from its inset.8, 9 Weinstock et al. demonstrated additional benefit of the buccal flap covering the BFP over the graft. GTR membrane which was secured on the BFP acts as a physical barrier between BFP and the bone graft which helps in mucosalisation of BFP.
The application of sticky bone over the GTR membrane facilitates new bone formation and enhances wound healing. Its mouldable nature allows for easy shaping, handling, and prevents dispersion. Furthermore, the presence of enriched growth factors in i-Platelet Rich Fibrin (PRF) contributes to a positive effect on both new bone formation and soft tissue healing.10 Additionally, securing a collagen membrane over the sticky bone prevents graft dislodgment and provides supplementary support.
Conclusion
Effective OAF closure is vital to prevent maxillary sinus-related complications, especially concerning future implant rehabilitation. Combining soft tissue and hard tissue techniques, such as BFP and bone grafting, with buccal advancement flap support, offers a comprehensive approach to OAF closure. The three layered approach described in this case report demonstrates excellent clinical outcomes with minimal postoperative discomfort and preserved vestibular architecture. While further research is warranted, this technique presents a valuable addition to the existing repertoire of OAF closure methods.