Introduction
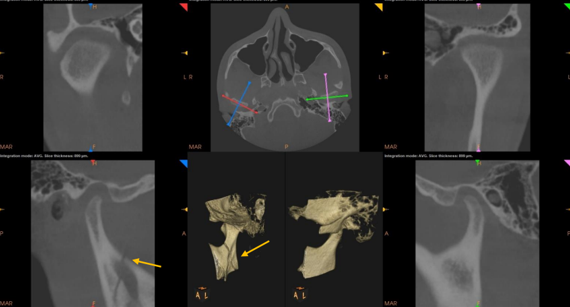
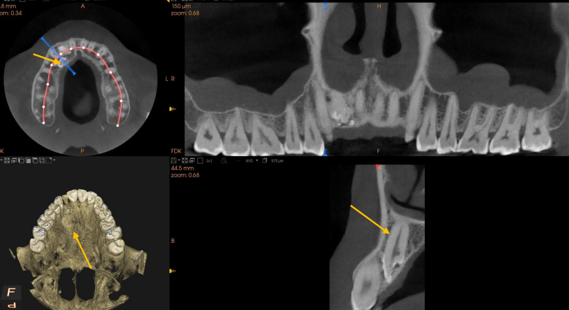
Cone-beam computed tomography (CBCT)(Figure 1) is a form of sectional imaging modality that allows precise three - dimensional mapping of hard tissue structures. It is also known by few other names like C-arm CT, cone-beam volumetric CT, flat- panel CT, or volumetric digital tomography (DVT). CBCT is the most important imaging modality among recent developments in medical diagnostic imaging technology.1
Apart from the sectional images obtained, CBCT has added advantage of lesser radiation dose.2 The sectional images ensure apt visualization of microstructure of tooth and or skeletal hard structures with very little distortion.
CBCT has wide range of applications in various fields of dentistry ranging from assessment of impacted teeth position, diagnosing airway lesions, assessment of root position and structure, surgical planning, temporomandibular joint assessment, assessment of skeletal asymmetry, and mini-screw placement etc. 2
CBCT can be used to generate both static 3D images and rotational reconstructions. Static 3D images can provide detailed information about a specific location, while 3D rotating images can be rotated from any direction.2 (Figure 1)
With this wide range of applications, CBCT has revolutionized imaging in dentistry, providing clinicians with a valuable tool for accurate diagnosis and treatment planning.
Aims and Objectives
The objective of the present paper is to highlight the existing and emerging role of integration of CBCT in interdisciplinary diagnosis and treatment planning in various fields of dentistry.
Basic Principles of CBCT
Field of view (FOV)
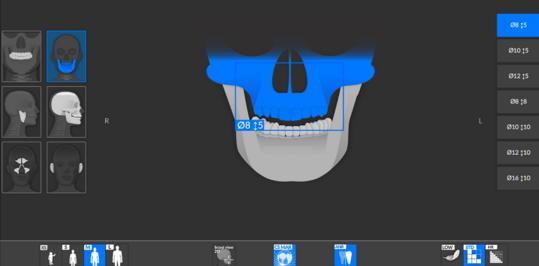
The size of the FOV describes the scan volume of a particular CBCT and depends on the size and shape of the transducer, beam projection geometry, and beam collimation capability. Beam collimation limits the patient's exposure to ionizing radiation and ensures that the appropriate FOV can be selected on a case-by-case basis. (Figure 2, Figure 3) In general, CBCT units can be classified into small, medium, and large based on their field of view size. Small volume CBCT machines are used to scan a quadrant to a single jaw. They generally provide higher image resolution because X-ray scattering (noise) decreases as the FOV decreases. The medium volume CBCT machine is used to scan both jaws, while the large FOV machine that allows full head visualization is commonly used in orthodontic and orthopedic surgical treatment planning. 3
The images obtained with right FOVs can be oriented according to the assessments intended. 3
The scan volume limit is based on required analysis by the clinician. For most dental implant applications, a small or medium field of view is sufficient to visualize the structures. Small volume CBCTs are more popular in endodontic cases due to increased spatial resolution, reduced patient radiation exposure, smaller volume to be interpreted. 3
Various Applications of CBCT
The introduction of CBCT has revolutionized the way an oral physician and maxillofacial radiologist’s perspective of diagnosing pathologies. With the inherent advantages such as being compact, cost-effective, 3D evaluation and low radiation exposure alternative to medical computed tomography, it has found its place for diagnosing various lesions.
The plethora of possibilities include - assessment of paranasal sinuses, airway analysis evaluation of temporomandibular joints, pathological lesions of the jaw, fractures of dento-maxillofacial structures, diagnosis malignant lesions to name a few. 4
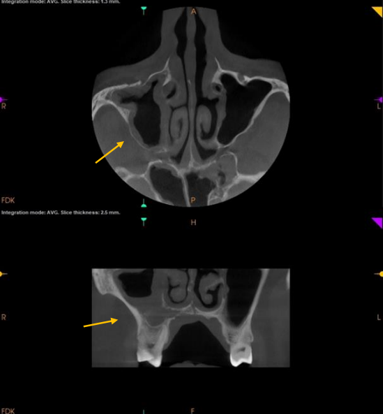
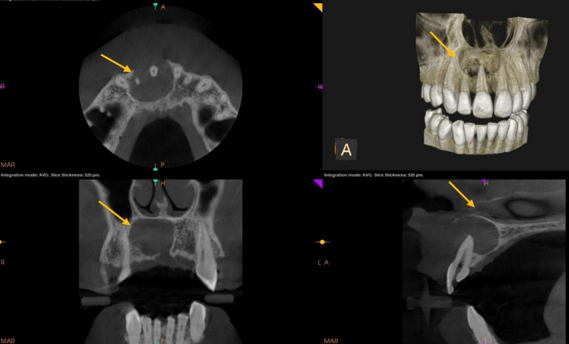
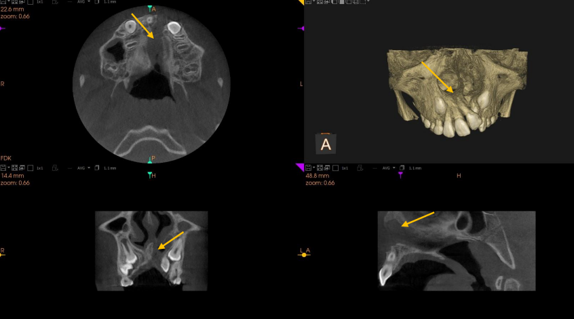
For the evaluation of paranasal sinuses, (ethmoid, sphenoid, frontal, and maxillary) CBCT images provide details such internal structural changes such as mucosal thickening, osseous changes, proximity to the maxillary alveolus, presence of foreign objects, and even odontogenic processes. (Figure 4)
Airway analysis
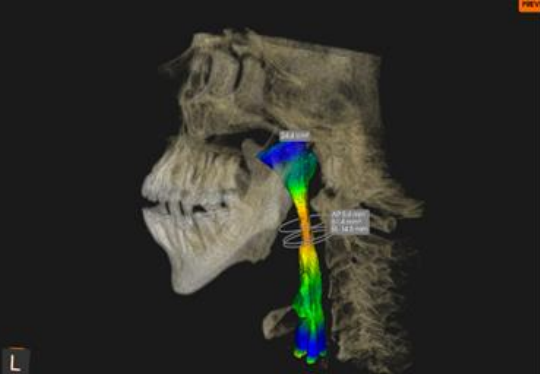
The airway space includes the nasal cavity, nasopharynx, velopharynx, oropharynx, and hypopharynx. Large FOV CBCT can be utilized to evaluate this entire space.
Although polysomnography is the confirmatory modality to establish the diagnosis of obstructive sleep apnea (OSA), CBCT can be aid as early diagnostic aids in establishing either sleep disordered breathing or OSA. Also, CBCT can help identify patients who are predisposed to these conditions.5, 6
CBCT scans only offer a static image of the airway space assisting in the detection of anatomical or pathological alterations. (Fig 5) The airway space should be examined for patency and symmetry, quantification of airway measurements or assist for developing 3D models.5, 6
CBCT can also aid in planning prior to orthognathic surgery, an airway examination may be conducted for volumetric measures, and surgical treatment options can be evaluated based on the severity of the jaw position. 5
Temporomandibular joints (TMJs)
CBCT scan of the TMJs provide details of osseous abnormalities in the mandibular condyle or glenoid fossa of the temporal bone. Osseous changes such as Trauma/fracture, (Figure 6) degenerative alterations, or neoplastic processes are well depicted. The only drawback with respect to TMJ is that the disc position cannot be evaluated.6, 7 In addition the condylar inclination can be assessed on CBCT for incorporation in virtual planning for prosthetic rehabilitations.6, 7, 8
Pathological Lesions of Jaw
CBCT scans majorly contribute in detailed assessments of various pathologies like cysts and benign jaw tumors, depicting the complete extent of the lesion as well as the impacts on critical neighboring structures. (Figure 7) It will also assist in designing the surgical approach.3
Fractures of Dento-Maxillofacial Structures
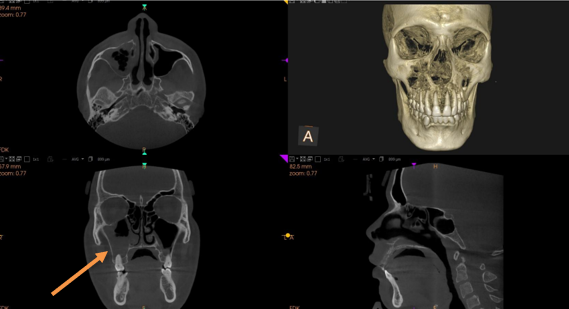
Periapical or panoramic radiographs can be used to diagnose a simple dental or jaw fracture. Plain films can also be used to assess the severity of a complex jaw fracture. However, CBCT images may be more useful in evaluating multiple jaw fractures with bone displacement. (Figure 8) CBCT images stand out to be far more superior to periapical radiographs for identifying root fractures. Considering radiation dose and image quality, CBCT stands out as a viable alternative imaging method to Computed tomography (CT) for analysis of complex jaw fractures including diagnosis of non-displaced fractures of the mandibular condyle, and condylar head interarticular fractures. 9
CBCT in mucormycosis
CT is the preferred mode of investigation in most cases of mucormycosis to identify the extension of lesion in Rhino maxillary area. (Fig 9) CBCT, produces images comparable to medical CT at lower costs and radiation doses. In many cases, CBCT has been deemed the examination of choice because it provides high resolution imaging, diagnostic consistency, and risk benefit assessment. 10
CBCT in orthodontics and dentofacial orthopedics
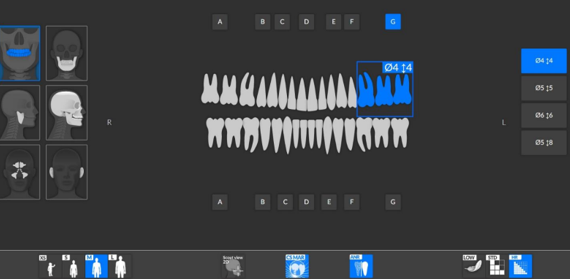
CBCT has many applications, which include assessment of bone for Temporary anchorage device (TAD) placement, Treatment outcomes. Evaluation of cervical vertebral maturation (CVM), and in assessment of bone/ site for auto-transplantation of teeth, assessment of status of impacted and transposed teeth.
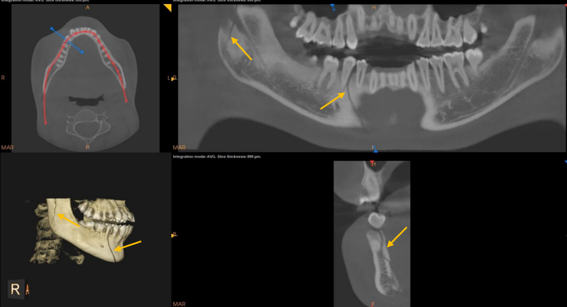
Among the impacted teeth, needing evaluations prior to orthodontic treatment, Maxillary canines are second in common for impacted teeth after third molars. 11 Use of traditional radiographs for assessments will need use of multiple radiographs in different directions.
CBCT improves the ability to accurately localize impacted teeth and assess their proximity to other teeth and structures, as well as to determine the alveolar width, the presence of pathology, and the rate of root resorption of neighboring teeth. (Fig 10) It also helps in the planning of surgical access and bond placement, as well as in determining the best direction for the extrusion of these teeth into the oral cavity.
For impacted teeth, it would be possible to ascertain precisely the position of the tooth, presence of dilacerated root, alveolar boundary conditions if exposure or forced eruption is planned. Using CBCT increases the clinician's confidence in the diagnosis and treatment plan as it helps to specify the surgical access site, the bond location, and the design of mechanics. 12 with the advent of AI in software it’s also possible to move the teeth virtually in the planned position. 12
The most prevalent craniofacial defect in humans is cleft lip and palate. 11 Preoperative CBCT imaging may enable visualization of the three-dimensional morphology of the bone and the relationship between the bone and roots of the neighboring teeth (Figure 11 ). It may also help in the appropriate selection of an autogenous graft donor site before surgery.
Maxillary Transverse Dimension and Maxillary Expansion
CBCT aids in precisely assessing transverse dimension determining the requirement for transverse maxillary expansion.
CBCT for periodontal conditions
CBCT aids various aspects for diagnosis and treatment evaluation of periodontal structures. These include assessment of lamina dura, periodontal ligament Space (PDL), assessment of alveolar bone defect, evaluation of furcation involvement & in implant planning. Accurate PDL space surveillance will hint occlusal trauma diagnosis and also will aid in understanding the effect of systemic disorders on the periodontium. 13, 14
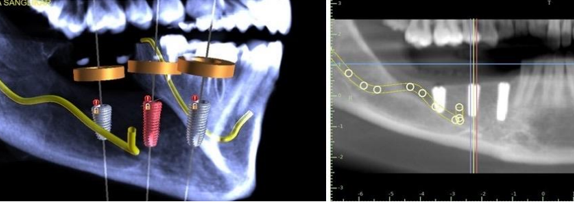
CBCT For implant planning15
The growing inclination for the selection of dental implants as a viable alternative to replace missing teeth has necessitated a reliable technique capable of obtaining highly accurate measurements to avoid likely damage to neurovascular and vital structures during implant surgery. CBCT has crucial role in assessing Anatomic structures such as the inferior alveolar nerve, maxillary sinus, mental foramen. Further, the specific CBCT images permit precise measurement of distance, area.
The detailed analysis using the soft wares help, an implantologist to can gain confidence in treatment planning for complex surgical procedures such as sinus lift and ridge augmentation. CBCT also has role in aiding in virtual planning of implants and fabrication of the surgical guides. (Figure 12)
Maxillo facial prosthodontics
DICOM data from CBCT can be used to create 3D augmented virtual models of the patient’s face, bony structures, and dentition. The shape of the graft can be virtually planned and can also be positioned in the defect creating a virtual reconstruction of the defect prior to the actual surgery. In addition, implant placement (if required) onto the graft can also be planned. Obturators for cleft closures can be precisely milled in larger CAD/CAM units, thereby eliminating the entire cumbersome clinical process of obturator construction.6
Discussion
The advent of cone-beam computed tomography (CBCT) has significantly transformed the diagnostic capabilities of oral physicians and maxillofacial radiologists. Its advantages, including compact size, cost-effectiveness, three-dimensional (3D) evaluation, and low radiation exposure, make it a valuable alternative to traditional medical CT, particularly in the assessment of dento-maxillofacial structures.4
This discussion highlights the broad range of CBCT applications across various maxillofacial and dental specialties.
CBCT offers detailed visualization of the paranasal sinuses, providing critical insight into mucosal thickening, osseous changes, and other internal structural alterations. It serves as a valuable tool for diagnosing sinus pathologies and odontogenic processes that extend into the sinuses. When assessing these structures, CBCT provides precise information about the proximity of foreign objects or the maxillary alveolus, facilitating pre-surgical planning or treatment decisions.4, 5
In airway analysis, particularly for conditions like obstructive sleep apnea (OSA), CBCT plays a supplementary diagnostic role. While polysomnography remains the gold standard for diagnosing OSA, CBCT can provide valuable early insights into anatomical predispositions for sleep-disordered breathing. CBCT’s 3D imaging helps evaluate the airway's patency and symmetry, offering volumetric measurements that assist in identifying airway obstruction before corrective procedures, such as orthognathic surgery.5, 6
The ability of CBCT to provide high-resolution imaging of the temporomandibular joints (TMJs) enhances diagnostic precision for osseous changes such as trauma, degenerative conditions, or neoplastic growths.6, 7, 8 Despite its inability to assess disc positioning, CBCT provides crucial details of the mandibular condyle and glenoid fossa. This is essential for diagnosing TMJ disorders, aiding in surgical planning, and determining prosthetic rehabilitation approaches by assessing condylar inclination.
One of the most critical applications of CBCT is its ability to evaluate pathological lesions of the jaw, such as cysts or benign tumours. 3 With its superior 3D imaging capabilities, CBCT allows clinicians to determine the lesion's full extent and its relationship with adjacent structures.
This information is instrumental in designing an effective surgical approach, minimizing complications, and improving patient outcomes.
For fractures of dento-maxillofacial structures, CBCT excels in identifying complex fractures, particularly in cases where displacement of bone segments or multiple fractures exist.9 Compared to periapical or panoramic radiographs, CBCT provides higher resolution and more comprehensive visualization, especially in non-displaced fractures of the mandibular condyle and other complex fractures.
In orthodontics and dentofacial orthopaedics, CBCT has revolutionized treatment planning and outcomes assessment. By providing accurate localization of impacted teeth, such as maxillary canines, CBCT helps orthodontists avoid complications during treatment. It aids in planning surgical approaches, determining bond placement, and deciding the best course of action for moving impacted teeth into alignment.11
Furthermore, CBCT imaging assists in evaluating the bone structure for temporary anchorage devices (TADs), bone graft donor sites, and craniofacial anomalies such as cleft lip and palate.11, 12
CBCT also plays a vital role in assessing the maxillary transverse dimension and the need for maxillary expansion. For patients requiring implant placement, CBCT's detailed imaging ensures precise planning, helping avoid complications related to neurovascular structures like the inferior alveolar nerve and maxillary sinus. The ability to perform virtual planning using CBCT data significantly improves the predictability of implant surgeries and complex procedures such as sinus lifts and ridge augmentation. 13, 14
In maxillofacial prosthodontics, CBCT enables the creation of 3D virtual models for surgical planning, including grafting and defect reconstruction. This technology facilitates the pre-surgical design of obturators for cleft closures and prosthetics, streamlining the process and increasing accuracy through the use of CAD/CAM technology.6, 10
Finally, CBCT’s application extends into the diagnosis and treatment planning of periodontal conditions, allowing clinicians to assess periodontal ligament (PDL) space, alveolar bone defects, and furcation involvement with unparalleled clarity. CBCT imaging helps clinicians diagnose occlusal trauma, evaluate the impact of systemic disorders on periodontal health, and plan surgical interventions.13, 14
Conclusion
CBCT stands out as a sectional imaging modality depicting the accurate relationships between teeth and anatomical structures. It has a wide range of applications in almost all fields of dentistry. Even though it has many applications, its use has to be mandated when standard imaging is insufficient to evaluate a patient's oral health or treatment outcome.