- Visibility 104 Views
- Downloads 29 Downloads
- DOI 10.18231/j.johs.2024.025
-
CrossMark
- Citation
A clinical prospective study on the surgical management of zygomatico-maxillary complex fractures using two-point fixation
- Author Details:
-
K N Abhinandan Patel
-
Kora Ramya Reddy *
-
G Girish
-
TR Sneha
-
G Nikhila
Introduction
The zygomatico- maxillary complex (ZMC) is the main buttress of the middle third of the facial skeleton , forming the lateral projection of the face.[1], [2], [3] Due to its position and contour it is the second most common mid face fractures ,first being the nasal bone.[4]
Failure of recognition and improper management these injuries may result in not only functional morbidity but also significant cosmetic defect.[1], [5]
The main objective of the management of ZMC fractures is to obtain anatomic reduction and fixation in order to prevent post-operative deficit. There are numerous theories and clinical studies of treatment options which are debatable as to which is better than the other. Right from a single point fixation to four point fixation of ZMC fracture depending on the type of fracture, displacement of the complex and stability of the zygomatic arch after reduction. [1], [5], [6], [7] Although each techniques has its own advantages, it also has various complications which could be avoided with a simpler and easier management technique.
This aim of this study was to evaluate the efficacy of two point internal fixation using conventional miniplates and screws at the zygomatic buttress and the fronto zygomatic suture. after evaluating both clinically and radiographically. Assessment was done both clinically and radiographically for stability and alignment post operatively.
Materials and Methods
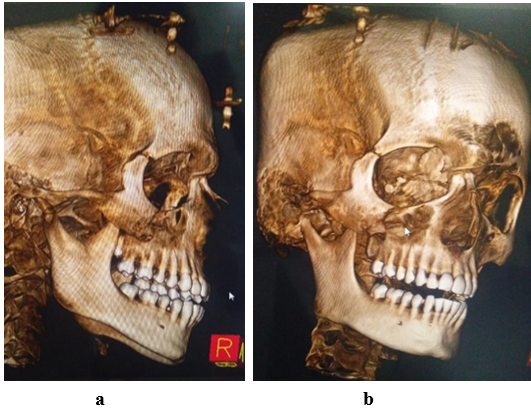
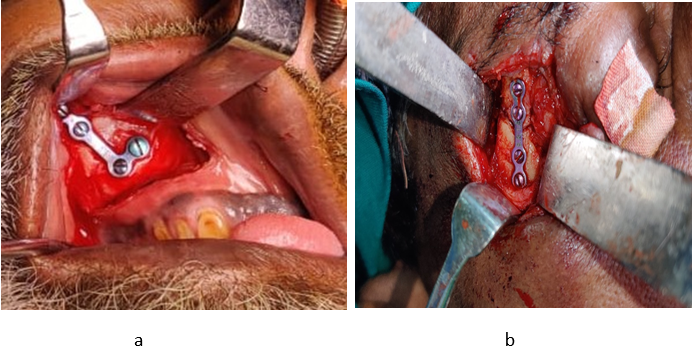
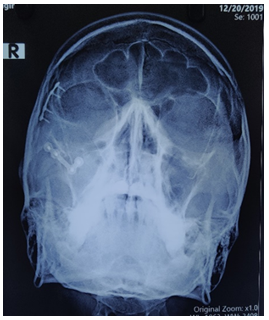
A prospective study was conducted on 35 patients with confirmed clinical and radiographic diagnosis of ZMC fracture reported to the department of facio-maxillary surgery, in our institute from the month of October 2019 to March 2020. The inclusion criteria were: patients with unilateral isolated ZMC fractures that required open reduction and internal fixation, age between 18-60 years irrespective of gender, the exclusion criteria was- patients with pre-existing medical conditions, infected fracture site, patients who were treated by conservative management and those who were not willing to participate in the study. Ethical clearance for the study was obtained from the ethical committee (Date of approval- 15/10/2019) and adheres to the guidelines. Written informed consent was taken from all the patients and were operated under general anesthesia following routine hematological, biochemical, general physical examination and routine radiographic examination ([Figure 1] (a) and (b)). Intra-oral vestibular approach was carried out for the buttress while an extra-oral lateral eyebrow incision was used for the FZ region. All fractures were reduced and fixation was done at two points – maxillary buttress ([Figure 2] (a)) and at fronto-zygomatic(FZ) suture ([Figure 2] (b)], with a 2mm ‘L’ shaped plate and 1.5mm 4 hole with gap miniplates respectively. Post- operatively patients were assessed clinically and radiographically using post op PNS view ([Figure 3]) at the follow up intervals of 1st, 3rd and 6th week. Charts of patients were reviewed for age, gender, etiology, malar height analysis and vertical dystopia.
Malar height Analysis –the malar was measured by using a Vernier caliper, preoperatively from the vertex view of the patient comparing fractured site with normal site. One point i.e. the reference point intersection of the midsagittal line with the intercanthal line was taken and the second point was taken at the maximum height of malar region as viewed from vertex view.
Vertical orbital dystopia – This again was measured preoperatively and postoperatively as the difference in the level of bony orbits indicated by both palpation and comparing it with the normal side measured by a steel scale on paranasal sinus view radiograph using a tracing sheet to outline the infraorbital margin.
Result
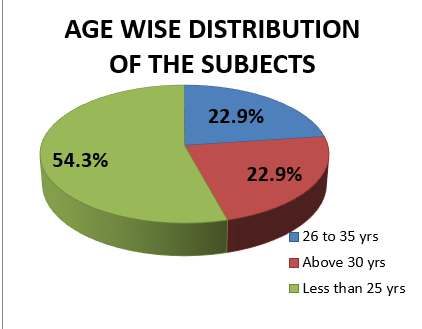
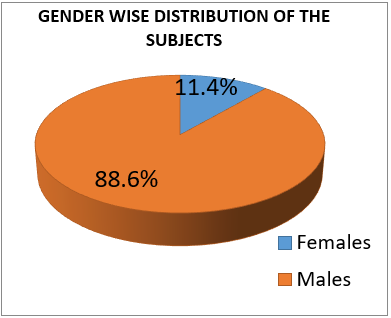
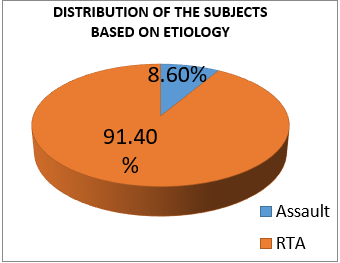
There were a total of 35 patients with ZMC fractures who underwent ORIF under GA with two-point fixation. The mean age was 26.37 with a standard deviation of 6.179. Among the age distribution it was noted that maximum number of cases were seen in the age group less than 25yrs of age 19 (54.3%). {[Table 1], [Figure 4]} Male patients formed a majority 31 (88.6). ([Figure 5]) The main etiology of the injury was RTA 34 (91.4%) while assault constituted the rest, 4 (8.6%). ([Figure 6])
Malar height analysis
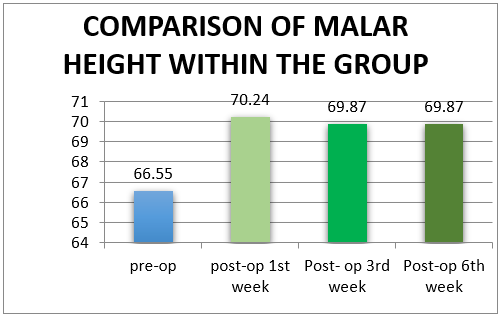
Preoperatively, mean malar height ± standard deviation of the patients recorded was 66.55 ± 3.02. Postoperatively, at the 1st week, value recorded was 70.24 ± 2.05, but in the 3rd and 6th weeks, it was the same, i.e. 69.87 ± 1.98 [[Table 2] , [Figure 7]]. There was a significant increase in malar height postoperatively (P < 0.0001).
Mean vertical dystopia
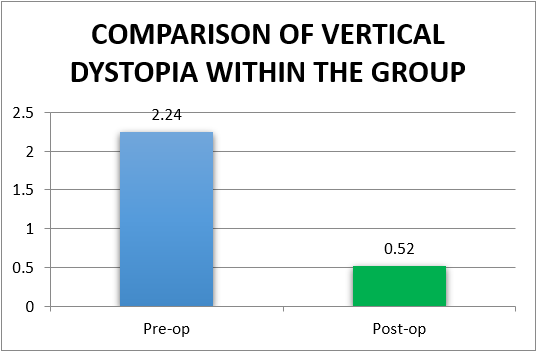
Preoperatively, mean vertical dystopia ± standard deviation of patients recorded was 2.24 ± 0.71 postoperatively, 0.52 ± 0.52 value was recorded. ([Table 3], [Figure 8]). Postoperative resolution of vertical dystopia was statistically significant (P<0.0001).
The study was analyzed using SPSS [statistical package for social sciences] software V.22, IBM.Corp. the mean and Standard deviation was compared within pre and post operatively using ANOVA test followed by post-hoc bonferroni test.
|
Age- classified |
Frequency |
Percent |
|
26 to 35 yrs |
8 |
22.9 |
|
Above 30 yrs |
8 |
22.9 |
|
Less than 25 yrs |
19 |
54.3 |
|
Total |
35 |
100.0 |
|
Malar Height analysis |
Minimum |
Maximum |
Mean |
Std. Deviation |
P value |
|
pre-op |
61.50 |
71.25 |
66.55 |
3.02 |
0.00* |
|
post-op 1st week |
65.30 |
73.60 |
70.24 |
2.05 |
|
|
Post- op 3rd week |
64.50 |
73.40 |
69.87 |
1.98 |
|
|
Post-op 6th week |
64.50 |
73.40 |
69.87 |
1.98 |
|
Vertical Dystopia |
Minimum |
Maximum |
Mean |
Std. Deviation |
Mean diff |
P value |
|
Pre-op |
1.30 |
4.00 |
2.24 |
.71 |
1.72 |
0.00* |
|
Post-op |
.00 |
1.50 |
.52 |
.33 |
Discussion
The integrity of the zygomactico-maxillary complex is well established as an important aspect in the maintenance of normal facial width and prominence of the cheek.[8], [1] Due to its lateral prominence, it is commonly injured, the most common etiology being road traffic accidents followed by interpersonal violence.[1], [9] Hence it is the second most common mid-facial bone fractured after the nasal bones and overall represents 13% of all craniofacial fractures. These ZMC fractures result in both functional (diplopia, trismus, and paresthesia) and also aesthetic deformities (mid-facial widening, malar flattening and globe malposition).
Over the years a lot of light has been shed on the various points of fixation for these fractures, each having their own reasoning to do so. Thus our intention was to assess the efficacy and the stability of two‑point fixation (buttress and FZ) in the management of isolated unilateral displaced ZMC fractures. In the present study, out of the 35 patients included, ZMC fractures were observed in the age group of 18 to 42 yrs. and higher incidence was noted in the age group less than 25 yrs. The main etiology observed in our study was RTA 91.4%, this finding was in agreement with Edward Ellis et al and Singaram et al.[4], [10] Ozoemene Obuekwe et al.[11] This could be due to various reasons such as inadequate road safety awareness, use of alcohol or substance abuse, speed limit violation. Our study consisted of 88.6% percent of males and 11.4% of females. This was attributed to the fact that men are more prone to indulge in reckless driving and engaging in interpersonal violence.
The surgical management of ZMC fractures vary from surgeon to surgeon and also depends on factors such as the type of fracture and circumstance. In our study we used the intraoral maxillary vestibular approach and lateral eyebrow approach for the buttress and the FZ region respectively. In studies conducted by Ellis and Kittidumkerng, have assessed various treatment options for ZMC fractures in which it was noted that a combination of approaches was used, of which the intraoral vestibular incision and lateral eyebrow incision were the most commonly used approaches. [12] Another study conducted by Candamourty et al also discusses the various modalities for surgical management, this correlates with our study regarding the approach to the ZMC fractures and also highlights the complications with the lower eyelid incision and infraorbital incisions i.e. scleral show and prominent scar respectively. [13] In our study they were no significant complications associated with maxillary vestibular approach or the lateral eyebrow approach. Chuong and Kaban in their study recommended that the lateral eyebrow approach is preferred for the initial access to the fronto-zygomatic region, as it not only provides direct access to the FZ suture but also has the advantage of producing an inconspicuous scar. They noted that there were no specific complications and it also provided a better long‑term esthetic result. [14] Our study also exhibited the same results where lateral eyebrow approach was the second prime approach following the vestibular approach for all of our cases.
ElSheikh et al in their study of comparison between 2 point and 3-point fixation stated that although 3-point fixation is known to exert maximum stability, the results of their clinical comparative study revealed that there was no significant difference in between the two groups regarding most of the parameter used including patient satisfaction was similar in both groups. They also mentioned that in addition to an extra point of fixation, the cost and the duration of the surgery also increases. [15]
A study conducted by Scott J. Farber, talks about the different types of fractures and their fixation and says that fixation highly depends on the type of fracture and can include immobilizing and any combination or single point of fixation. The main sites being FZ suture, ZM buttress, inferior orbital rim, zygomaticosphenoid suture, and zygomatic arch. They also mention about the misconception that, although it seems obvious that increase in points of fixation leads to increase in stability, isn’t entirely true for all fractures. They go on to conclude that ZMC fracture treatment should be tailored on a patient-by-patient basis.[6]
Various authors over the years have proposed that 2-point fixation using a miniplate conferred a degree of stability comparable with most methods of 3-point fixation, regardless of the site at which the miniplates were fixed. Many studies such as one conducted by O Hara et al and also Lee et al have observed that zygomatico-maxillary buttress is one of the best site for fixation in ZMC fractures because it is direct antagonist to the pull of masseter muscle and site of fixation is in an unpalpable area thus making it a strong point for fixation. [16], [17] They also showed that, although FZ was having the best bone for fixation but it was the worst single-alignment guide. It can be used as a second or third area of evaluation.
Vertical orbital dystopia was measured as the difference in the level of bony orbits on PNS radiograph while the malar height was measured from the vertex view, comparing between fractured site and normal site. According to a study conducted by Rana et al. with average malar height in two‑point fixation being 66.72 ± 3.62 mm with minimum and maximum value of 59 mm and 75 mm, while the average malar height in three‑point fixation being 68.26 ± 3.76 mm with minimum and maximum value of 60 mm and 74 mm. The average vertical dystopia in two‑point fixation was 3.18 ± 1.003 mm with a range of 4 mm and in three‑point fixation average vertical dystopia was 2.36 ± 1.102 mm with a range of 3 mm.[9]
In our study, mean malar height ± standard deviation of the patients recorded was 66.55 ± 3.02 was recorded on the normal side, preoperatively. Postoperatively, at 1st week, value recorded was 70.24 ± 2.05, but in the 3rd and 6th weeks, it was the same, i.e. 69.87 ± 1.9, suggesting a significant increase in malar height postoperatively.
These results were in agreement to a study conducted by Mittal et al in which they noted that preoperatively the mean malar height recorded was 66.45 ± 4.67 mm, while postoperatively value recorded was 69.10 ± 4.35 mm, which was statistically significantly. The vertical dystopia measured pre-operatively was 2.85 ± 1.27 mm, while postoperatively, mean vertical dystopia was 0.28 ± 0.55 mm, which was also statistically significant.[18]
Limitation
The sample size considered for the study is limited and the follow-up duration was confined to only 6weeks. Further research over a larger group of patients over a longer time span to be carried out.
Conclusion
In our study, all patients that were treated with two‑point fixation showed satisfactory results both functionally and esthetically. This technique of two-point fixation also provides an additional advantage over the three-point fixation by eliminating the need for opening up another surgical site, saving time and cost of the surgery and most importantly the external scar at infraorbital rim along with the complication that arise with it. There by we conclude that our study thus provides a basis for more research with a larger sample size and a longer follow‑up period to further emphasis and to prove the efficacy of two‑point fixation when compared to single‑ and three‑point fixation techniques.
Source of Funding
None.
Conflict of Interest
None.
References
- N Gadkari, S Bawane, R Chopra, K Bhate, D Kulkarni. Comparative evaluation of 2-point vs 3-point fixation in the treatment of zygomaticomaxillary complex fractures - A systematic review. J Cranio-Maxillofac Sur 2019. [Google Scholar]
- D Bradley, B Leung, S Saxena, M Dungarwalla, D Chapireau, K Fan. Surgical management of zygomatic complex fractures in a major trauma centre. Plast Aesthetic Res 2019. [Google Scholar]
- J Sy, SS Kim, MH Kim, WS Yang. Surgical Methods of Zygomaticomaxillary Complex Fracture. Arch Craniofac Surg 2016. [Google Scholar]
- E Ellis, A El-Attar, KF Moos. An Analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg 1985. [Google Scholar]
- M Marinho, RO Freire-Maia. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin North Am 2013. [Google Scholar]
- SJ Farber, DC Nguyen, GB Skolnick, AS Woo, KB Patel. Current Management of Zygomaticomaxillary Complex Fractures: A Multidisciplinary Survey and Literature Review. Craniomaxillofac Trauma Reconstr 2016. [Google Scholar]
- R Vatsa, P Priyadarshini, AD Bhagat. Comparison of One Point Fixation Vs Two Point Fixation in the Treatment of Zygomatico Maxillary Complex Fractures. Int Healthc Res J 2018. [Google Scholar]
- B Yamsani, R Gaddipati, N Vura, S Ramisetti, R Yamsani. Zygomaticomaxillary Complex Fractures: A Review of 101 Cases. J Maxillofac Oral Surg 2016. [Google Scholar]
- M Rana, R Warraich, S Tahir, A Iqbal, C Von See, A M Eckardt. Surgical treatment of zygomatic bone fracture using two points fixation versus three point fixation-a randomised prospective clinical trial. Trials 2012. [Google Scholar]
- M Singaram, G Sv, RK Udhayakumar. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. J Korean Assoc Oral Maxillofaurgc 2016. [Google Scholar]
- O Obuekwe, F Owotade, O Osaiyuwu. Etiology and pattern of zygomatic complex fractures: A retrospective study. J Natl Med Assoc 2005. [Google Scholar]
- E Ellis, W Kittidumkerng. Analysis of treatment for isolated zygomaticomaxillary complex fractures. J Oral Maxillofac Surg 1996. [Google Scholar]
- R Candamourthy, V Narayanan, MF Baig, MR Muthusekar, MK Jain, RM Babu. Treatment modalities in Zygomatic complex fractures: a prospective short clinical study. Dent Med Res 2013. [Google Scholar]
- R Chuong, LB Kaban. Fractures of the Zygomatic complex. J Oral Maxillofac Surg 1986. [Google Scholar]
- WF Nasr, E Elsheikh, MW El-Anwar, AH Sweed, A Bessar, N Ezzeldin. Two- versus Three-Point Internal Fixation of Displaced Zygomaticomaxillary Complex Fractures. Craniomaxillofac Trauma Reconstr 2018. [Google Scholar]
- DE O’hara, DA Delvecchio, SP Bartlett, LA Whitaker. The role of microfixation in malar fractures: A quantitative biophysical study. Plast Reconstr Surg 1996. [Google Scholar]
- E Lee, K Mohan, J Koshy, L Hollier. Optimizing the Surgical Management of Zygomaticomaxillary Complex Fractures. Semin Plast Surg 2010. [Google Scholar]
- G Mittal, R Garg, S Sharma, RV Chhabra Rathi, G Ranjan. Efficacy of two-point fixation in the management of zygomatic complex fractures - A prospective clinical study. Nat J Maxillofac Surg 2019. [Google Scholar]
How to Cite This Article
Vancouver
Patel KNA, Reddy KR, Girish G, Sneha T, Nikhila G. A clinical prospective study on the surgical management of zygomatico-maxillary complex fractures using two-point fixation [Internet]. J Orofac Health Sci. 2024 [cited 2025 Sep 10];11(3):120-125. Available from: https://doi.org/10.18231/j.johs.2024.025
APA
Patel, K. N. A., Reddy, K. R., Girish, G., Sneha, T., Nikhila, G. (2024). A clinical prospective study on the surgical management of zygomatico-maxillary complex fractures using two-point fixation. J Orofac Health Sci, 11(3), 120-125. https://doi.org/10.18231/j.johs.2024.025
MLA
Patel, K N Abhinandan, Reddy, Kora Ramya, Girish, G, Sneha, TR, Nikhila, G. "A clinical prospective study on the surgical management of zygomatico-maxillary complex fractures using two-point fixation." J Orofac Health Sci, vol. 11, no. 3, 2024, pp. 120-125. https://doi.org/10.18231/j.johs.2024.025
Chicago
Patel, K. N. A., Reddy, K. R., Girish, G., Sneha, T., Nikhila, G.. "A clinical prospective study on the surgical management of zygomatico-maxillary complex fractures using two-point fixation." J Orofac Health Sci 11, no. 3 (2024): 120-125. https://doi.org/10.18231/j.johs.2024.025
