Introduction
Peripheral Giant Cell Granuloma (PGCG) is a frequently encountered benign lesion that occurs in the oral cavity.1 It typically arises from the gingiva or alveolar mucosa and presents as a soft tissue mass. PGCG often manifests as a painless, slowly growing swelling, ranging in colour from pink to red or bluish-purple.2 Peripheral Giant Cell Granuloma (PGCG) stands out as the most prevalent among oral giant cell lesions, characterized by a purplish-red extra-osseous soft tissue nodule. Originating from diverse oral structures such as the gingival connective tissue, periodontal membrane, or periosteum of the alveolar ridge, PGCG is believed to be a reactive lesion rather than a true neoplasm.3 While its initial stimulation is often attributed to local trauma or irritation, the precise mechanism remains elusive. Despite being termed a peripheral giant cell "reparative" granuloma, its actual reparative potential lacks definitive evidence.4 PGCG is observed across all age groups but predominantly affects individuals between 30 and 40 years, with a higher incidence among females (60%).5 Notably, the mandible is more commonly affected than the maxilla. Some lesions can attain considerable size, with diameters reaching up to 2 cm. While PGCG typically exhibits a bluish-purple hue rather than the bright red of a typical pyogenic granuloma, its clinical appearance often resembles that of pyogenic granuloma.6, 7 Differential diagnosis of Peripheral Giant Cell Granuloma (PGCG) involves distinguishing it from several other oral lesions that share similar clinical and radiographic characteristics.8 These include Pyogenic Granuloma, characterized by vascular proliferation without multinucleated giant cells, Fibrous Epulis presenting with dense fibrous connective tissue but lacking giant cells, and Peripheral Ossifying Fibroma exhibiting varying degrees of mineralization but without multinucleated giant cells. 9 Inflammatory Fibrous Hyperplasia, associated with chronic irritation, demonstrates fibroblastic proliferation and chronic inflammatory infiltrate, while Peripheral Odontogenic Fibroma consists of fibrous connective tissue and odontogenic epithelium without giant cells.10 Additionally, Papilloma presents with benign epithelial proliferation but lacks multinucleated giant cells. Histopathological examination remains crucial for definitive diagnosis, especially in cases where clinical and radiographic features overlap with other oral lesions, ensuring appropriate management strategies are implemented.11
Case Report
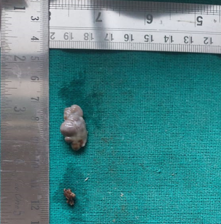
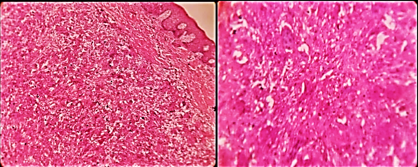
A female patient, aged 55, sought treatment at the Department of Periodontology within the School of Dental Sciences at Sharda University. complaining of swelling in the left upper jaw persisting for 2 months. Initially small, the swelling gradually enlarged over the two-month period and was accompanied by intermittent pain. The patient denied any history of trauma, neurological conditions, fever, decreased appetite, or weight loss, and was otherwise in good systemic health. Upon intraoral examination, a single prominent overgrowth was observed in the anterior maxilla on the left side of the face, measuring approximately 2 × 1 cm and located in relation to teeth 23 and 24 (Figure 1). The overgrowth appeared sessile, firm in consistency, and exhibited a bluish-red coloration. Intraoral periapical radiographs revealed bone resorption extending to the middle third of the root (Figure 2). The lesion was non-tender, with minimal to no bleeding. The patient demonstrated poor oral hygiene. Considering the relatively small size of the lesion, an excisional biopsy, followed by histopathologic evaluation, was recommended for definitive diagnosis. During the initial visit, thorough oral prophylaxis was performed, and the patient was advised to use 0.2% chlorhexidine mouthwash and warm saline rinses as postoperative care. Routine blood investigations were also advised. The patient was scheduled for the surgical procedure after one week. During the second visit, the surgical procedure was conducted under local anaesthesia (1:80000). The lesion was carefully isolated from the surrounding tissue and completely excised using a scalpel and blade no. 15. Gingival margins were contoured using Electrosurgery, and the surgical site was thoroughly irrigated with normal saline. Primary closure was achieved using 5-0 sutures. The excised specimen was promptly placed in 10% formalin and sent for histopathological examination of the biopsied specimen indicated that the tissue was firm in consistency, with a greyish-brown coloration, measuring 2.0cm x 1.0cm and preserved in 10% formalin (Figure 3). Upon staining with Haematoxylin and Eosin (H&E), the section revealed Para keratinized epithelium overlying the connective tissue stroma. Within the stroma, giant cells were observed along with dense collagen fibers interspersed with fibroblasts. Inflammatory cells, primarily lymphocytes with plasma cells, were also present, along with blood vessels. (Figure 4).
Postoperatively, the patient was instructed to refrain from eating or brushing in the surgical area for 24 hours. After this period, she was advised to rinse her mouth with 0.2% chlorhexidine mouthwash and warm saline rinses twice daily for a week. Additionally, medications including Amoxycillin (500mg) + Clavulanic acid (125mg), Aceclofenac (100mg) + Serratiopeptidase (15mg) + Paracetamol (325mg), and Pantoprazole sodium (40mg) were prescribed. The patient was scheduled for a follow-up visit and suture removal after one week. During the third visit, the sutures were removed, and the surgical area was irrigated with normal saline (Figure 5).
Discussion
Peripheral giant cell granuloma (PGCG) may present in both youthful and elderly populations, with the highest prevalence typically found between the 40th and 60th decades of life. 12 Nevertheless, it's noteworthy that approximately 20–30% of instances arise in the 1st and 2nd decades of life. 13 In the case detailed, the patient was 55 years of age. Regarding its location, while Pindborg observed a tendency for the premolar and molar areas, Shafer and Giansanti propose a heightened occurrence in the incisor and canine region. The exact cause and nature of PGCG remain elusive. Various theories have been proposed, including the suggestion that multinucleated giant cells are remnants of osteoclasts from normal tooth resorption or a response to periosteum injury. These cells have been shown to possess calcitonin receptors and osteoclast-like activity in vitro, supporting the theory of their osteoclastic origin. 14 Remarkably, although PGCG originates in soft tissue, it can cause superficial resorption of the alveolar bone crest, as evident in the intraoral periapical radiograph of the patient under consideration. The array of potential alternative diagnoses for PGCG includes pyogenic granuloma, fibrous epulis, peripheral ossifying fibroma, inflammatory fibrous hyperplasia, peripheral odontogenic fibroma, and papilloma. These conditions share similar clinical and radiographic features. Therefore, histological examination is crucial for a definitive diagnosis. Histopathological investigation of PGCG typically reveals ulcerative alterations in the epithelium, connective tissue with numerous small blood vessels, and multinucleated giant cells in the medullary or core area. These giant cells are surrounded by ovoid and spindle-shaped mesenchymal cells, and they can exhibit varying numbers of nuclei, ranging from few to several dozen. Studies on their ultrastructure and immune systems suggest their lineage from osteoclasts. 15
Conclusion
Peripheral Giant Cell Granuloma is recognized as one of the predominant oral giant cell lesions encountered in clinical practice. When opting for surgical intervention, it is imperative to address potential underlying causes and conduct thorough histological evaluations to ensure accurate diagnosis. Through a comprehensive approach encompassing clinical examination, radiographic imaging, and histopathological analysis, clinicians can achieve an early and definitive diagnosis of peripheral giant cell granuloma. This facilitates the implementation of conservative treatment strategies, thereby mitigating risks to adjacent hard tissues and promoting optimal patient outcomes.
This case study sheds light on the clinical presentation, diagnosis, and management of Peripheral Giant Cell Granuloma (PGCG), a common benign lesion encountered in the oral cavity. PGCG, often referred to as a "giant cell epulis," typically presents as a purplish-red nodule in soft tissue, with a background of mononuclear stromal cells, extravasated red blood cells, and multinucleated giant cells. While its exact etiology remains uncertain, PGCG is believed to be a reactive lesion rather than a true neoplasm, often triggered by local trauma or irritation.
In this case, a 55-year-old female patient presented with a swelling in the anterior maxilla persisting for two months. Clinical examination revealed a bluish-red overgrowth in the left maxillary region, accompanied by bone resorption evident on intraoral periapical radiographs. Differential diagnosis included several other oral lesions with similar clinical and radiographic features, highlighting the importance of histopathological examination for definitive diagnosis. Following excisional biopsy, histopathological evaluation confirmed the diagnosis of PGCG, revealing Para keratinized epithelium, multinucleated giant cells, dense collagen fibres, and inflammatory cells within the stroma. Surgical excision of the lesion was performed under local anaesthesia, followed by postoperative care and medication. The patient demonstrated satisfactory healing without persistent swelling or bone deformity during follow-up visits.
In conclusion, this case emphasizes the importance of accurate diagnosis and appropriate management strategies for PGCG to ensure optimal patient outcomes. Further research is warranted to elucidate the underlying mechanisms of PGCG and improve treatment approaches for this commonly encountered oral lesion.